Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Chronic Ankle Instability and Pain

Chronic ankle instability occurs when the ankle repeatedly gives out, often due to weakened ligaments from prior injuries like sprains. Over time, the ligaments fail to provide sufficient support, leading to instability and persistent pain. This condition is common in athletes and individuals who engage in activities involving quick turns or uneven surfaces. The pain typically feels like a dull ache or sharp twinge on the outer side of the ankle, often worsening with activity. Swelling, tenderness, and a sense of wobbliness may accompany the discomfort. Repeated instability can cause further injuries, cartilage damage, or arthritis. If you have chronic ankle stability, it is suggested that you see a podiatrist who can recommend treatments such as targeted exercises to strengthen the ankle, bracing for support, or, in severe cases, surgery.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with one of our podiatrists from Fusion Foot and Ankle. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our offices located in Fort Worth and Arlington, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Pain
Pain experienced in the ankle can be caused by a multitude of conditions. While the most common cause is an ankle sprain, other possible problems can include arthritis, gout, ankle instability, an ankle fracture, nerve compression, or tendinitis. In more serious cases, ankle pain can be a sign of improper alignment of the foot or an infection.
Ankle pain can often be accompanied by symptoms such as redness, swelling, stiffness, and warmth in the affected area. Pain can be described differently depending on the condition: short, stabbing pain and a dull ache are some examples. If such symptoms are persistent and do not improve after time, be sure to schedule an appointment with your local podiatrist.
Depending on the condition causing your ankle pain, different treatments may be prescribed by your podiatrist. For ankle sprains, the first step in treatment involves rest, ice, elevation, and compression. Be sure to avoid placing pressure on the ankle, use an ice pack several times a day, and use a compression bandage and elevation to reduce swelling. Other, more serious conditions may require the assistance of certain drugs and medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, or even cortisone injections.
Depending on the severity of your ankle pain and the condition behind it, recovery from ankle pain may take some time.
Consult with your foot and ankle doctor to best determine the cause of your ankle pain and the appropriate treatment.
Arthritis Can Cause Pain in the Feet and Ankles
Causes of a Broken Ankle

A broken ankle occurs when one or more bones in the ankle joint fracture due to trauma, falls, or twisting injuries. Symptoms include intense pain, swelling, bruising, inability to bear weight, and in severe cases visible deformity. Common causes include sports injuries, car accidents, or missteps on uneven surfaces. Treatment depends on the severity of the fracture. Minor breaks may only require a cast or boot, while complex fractures might need surgical intervention to realign the bones. Recovery typically takes six to twelve weeks, with targeted stretching exercises often necessary to restore strength and mobility. If you suspect a broken ankle, seek immediate care from a podiatrist especially if there is severe swelling, deformity, or numbness.
Broken ankles need immediate treatment. If you are seeking treatment, contact one of our podiatrists from Fusion Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our offices located in Fort Worth and Arlington, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Broken Ankle Causes, Differences, Symptoms and Treatments
The ankle is a hinged synovial joint made up of three bones: the tibia (shin bone), the fibula (outer ankle bone), and the talus (between the heel and leg). These three bones are bound, supported, and stabilized by strong, fibrous bands of tissue called ligaments.
A break in an ankle bone can be either traumatic or stress related. This injury may be referred to as a break or fracture. A traumatic fracture can result from tripping, twisting or rolling the ankle, falling, or by blunt impact to the ankle. These traumatic ankle breaks usually occur during sporting activities or accidents. Stress fractures, however, occur over time and are the result of repetitive stress to the ankle. These fractures sometimes occur when a new activity that engages the ankle is introduced, or when the level of activity is abruptly increased or intensified.
There are various symptoms that accompany an ankle break. The most significant symptoms are pain and swelling that occurs in the ankle and sometimes spreads up from the foot to below the knee. Bruising or discoloration may develop eventually. It will be difficult or even impossible to put weight on the affected foot, and in severe cases there may be a visible deformity or even exposed bone.
It is very important to seek immediate treatment when an ankle break occurs or is suspected to have occurred, in order to allow the bone to properly heal and to avoid future complications such as stiff joints, limited range of motion, and osteoarthritis.
To diagnose a broken ankle, your podiatrist will first ask you to explain how the injury occurred and what your symptoms are. They will perform a thorough examination, checking for damage to nerves, blood vessels, and other structures around the injury site. They will also test your range of motion. An X-ray will need to be reviewed and, in some cases, an MRI or CT scan may be necessary.
Proper treatment of a broken ankle will depend on where and how severe the break is, how stable the ankle is, and whether the bone is displaced (misaligned or separated) or non-displaced (broken yet still aligned properly).
Mild fractures (where the bone is non-displaced) may be treated by resting, icing, and elevating the ankle at first, followed by immobilization with a cast or walking boot. Pain and inflammation may be treated with acetaminophen. More severe or complicated fractures where bones or joints are displaced may require surgery.
Recovery time will also vary, and it may take 4-6 weeks or longer for a broken ankle to heal. Your podiatrist will most likely order progressive X-rays or stress tests to be taken in order to monitor the healing process.
Achilles Tendinopathy and How It Can Be Prevented

Achilles tendinopathy is a condition that affects the Achilles tendon, the large tendon at the back of the ankle that connects the calf muscles to the heel bone. It is often caused by repetitive strain, overuse, or sudden increases in activity, leading to pain, swelling, and stiffness. Athletes, particularly runners and those involved in high-impact sports, are at higher risk of developing this condition. To prevent Achilles tendinopathy, focus should be on exercises that strengthen the calf muscles, improve flexibility, and increase overall ankle stability. Eccentric strengthening exercises, which involve lengthening the tendon while under tension, are particularly effective in building tendon resilience. Additionally, gradual increases in activity levels, proper warm-ups, and wearing appropriate footwear can help reduce the strain on the Achilles tendon. Regular stretching, foam rolling, and cross-training can also prevent imbalances and reduce the risk of tendinopathy. If you have an Achilles tendon injury, it is suggested that you contact a podiatrist who can offer you treatment and relief solutions that are right for you.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Fusion Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Fort Worth and Arlington, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
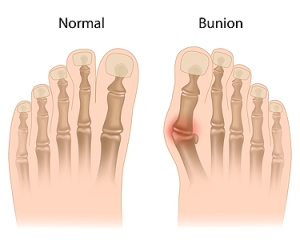
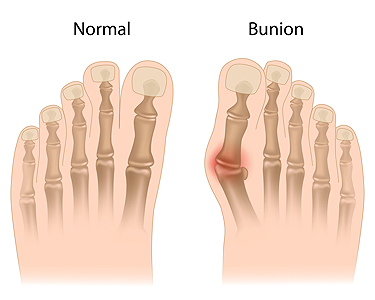
Understanding Bunions
A bunion is a bony bump that forms at the base of the big toe, causing it to angle inward toward the other toes. This condition can lead to pain, swelling, and redness surrounding the joint, making it difficult to find comfortable shoes. As the bunion develops, it can cause the toes to become misaligned, leading to additional discomfort and potential problems with walking. The primary cause of bunions is often hereditary, but wearing tight, narrow shoes, especially high heels, can make the condition worse. Foot deformities, such as flat feet, can also increase the risk. A podiatrist can help diagnose and manage bunions. Conservative treatments may include custom orthotics, padding, or recommending footwear changes to reduce pressure. In more severe cases, this type of doctor may suggest surgical options to realign the joint and alleviate pain. If you have developed a bunion, it is suggested that you schedule an appointment with a podiatrist.
If you are suffering from bunions, contact one of our podiatrists of Fusion Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our offices located in Fort Worth and Arlington, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.